Affirming mammography and primary care.
Research shows that due to past negative experiences with healthcare providers, LGBTQ+ individuals tend to delay regular health screenings, which results in later-stage cancer diagnoses and worse outcomes.
That’s why we’re training mammography staff across Ohio to provide culturally competent services to LGBTQ+ patients.

 ACCESS = LIFE
ACCESS = LIFE
Because early detection makes all the difference.
ACCORDING TO THE AMERICAN CANCER SOCIETY:
99% The 5-year relative survival rate for people with localized breast cancer
86% The 5-year relative survival rate for people diagnosed with regional breast cancer
28% The 5-year relative survival rate for people diagnosed with distant breast cancer
WHAT DO THESE CANCER STAGES MEAN:
Localized: No sign the cancer has spread outside of the breast.
Regional: The cancer has spread outside the breast to nearby structures or lymph nodes.
Distant: The cancer has spread to distant parts of the body such as the lungs, liver or bones.
Source: https://www.cancer.org
 ACCESS = INFORMATION
ACCESS = INFORMATION
Do LGBTQ+ people have a greater risk of breast cancer?
THE THREE MAIN RISK FACTORS FOR BREAST CANCER ARE:
1 Getting Older
2 Having Breast Tissue
3 Having a family history of breast cancer
There are no biological differences that put LGBTQ+ individuals at risk of breast cancer, but factors like discrimination, stigma, and isolation do impact health outcomes in our community.
Lesbian and bisexual cisgender women do experience breast cancer at higher rates than heterosexual cisgender women. Why?
In addition to factors like stress caused by stigma and isolation:
- Lesbians and bisexual women are more likely to put off regular mammograms due to previous negative experiences.
- Before the Affordable Care Act, many lesbians and bisexual women did not have insurance to cover the cost of preventative care. Lesbians and bisexual women are less likely to be pregnant or breastfeed, which reduce the risk of breast cancer.
- Lesbians and bisexual women have higher rates of smoking and obesity, which increase the risk of breast cancer.
 ACCESS = SELF CARE
ACCESS = SELF CARE
Breast Cancer Awareness Starts with You!
WHO
Lesbian, gay, bisexual, & trans women, trans men, and non-binary folks with breast tissue
WHEN
Ages 25-40
WHAT
KNOW YOUR BODY
Conduct monthly breast/chest self-exams (see last page of this booklet for instructions). If you notice any changes or anything unusual, call your doctor or nurse practitioner right away.
ATTEND REGULAR PHYSICALS
Schedule a well-check appointment with your doctor or nurse practitioner every year. They will check your breasts/chest for changes or concerns.
ASSESS YOUR RISK
Talk to your doctor or nurse practitioner about your breast cancer risk. A family history of breast cancer, a BMI greater than 35, and other factors increase your risk. Your doctor or nurse may recommend that you start mammograms before age 40.
PLEASE NOTE: The screening guidelines in this guide are for those of average risk for breast cancer.
 ACCESS = DIGNITY
ACCESS = DIGNITY
Screening Guidelines for Lesbian & Bisexual Cisgender Women
(of average risk)*.

Beginning at age 40:
Mammogram Recommended every year.
Physical With your doctor or nurse practitioner every year.
Self-Exam Breast/Chest Self-Exam every month.
*American College of Radiology Recommendations: Monticciolo DL, Newell MS, Hendrick RE, Helvie MA, Moy L, Monsees B, Kopans DB, Eby PR, Sickles EA. Breast Cancer Screening for Average-Risk Women: Recommendations From the ACR Commission on Breast Imaging. J Am Coll Radiol. 2017 Sep;14(9):1137-1143. doi: 10.1016/j. jacr.2017.06.001. Epub 2017 Jun 22. PMID: 28648873.
 ACCESS = VISIBILITY
ACCESS = VISIBILITY
Screening Guidelines for Trans Men and Non-Binary people with Breast Tissue (of average risk)*.
Those who have had chest reconstruction top surgery. Beginning at age 40:
Physical With your doctor or nurse practitioner every year.
Self-Exam Breast/Chest Self-Exam every month.
Those who have had breast reduction top surgery. Beginning at age 40:
Mammogram Recommended every year.
Physical With your doctor or nurse practitioner every year.
Self-Exam Breast/Chest Self-Exam every month.
Those who have not had top surgery. Beginning at age 40:
Mammogram Recommended every year.
Physical With your doctor or nurse practitioner every year.
Self-Exam Breast/Chest Self-Exam every month.
*UCSF Center for Transgender Excellence: https://transcare.ucsf.edu/guidelines/breast-cancer-men
 ACCESS = REPRESENTATION
ACCESS = REPRESENTATION
Screening Guidelines for Trans Women who have had 5 or more years of hormone replacement therapy*.

Beginning at age 50:
Mammogram Recommended every year.
Physical With your doctor or nurse practitioner every year.
Self-Exam Breast/Chest Self-Exam every month.
*UCSF Center for Transgender Excellence: https://transcare.ucsf.edu/guidelines/breast-cancer-women
 ACCESS = AFFORDABILITY
ACCESS = AFFORDABILITY
How do I pay for a mammogram or chest wall exam?
Payment for services depends on health insurance coverage. The Affordable Care Act requires insurers to cover the cost of breast tissue screenings for any patient who is at least 40 years old and any patient under 40 who has been referred by a primary care physician due to a family history of breast cancer or other risk factors.
 ACCESS = PREPARATION
ACCESS = PREPARATION
First Mammogram?
If you’ve never had a mammogram or chest wall exam, you may have a few questions.
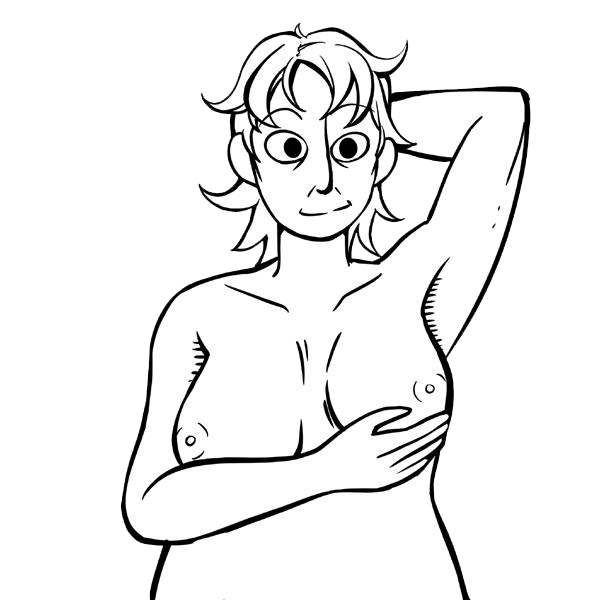
Standing Up
You will use the pads of your fingers to examine each breast or each side of your chest from your collarbone to your ribs.
- Starting in the middle of your armpit, make small circles with your fingertips. Make the circles going up and down the area, moving from top to bottom. Continue this motion all the way across to the middle of your chest.
- Feel for any lumps, thickening, or hardened knots.
Contact your doctor or nurse practitioner immediately if you detect any changes or abnormalities on your self-exam.
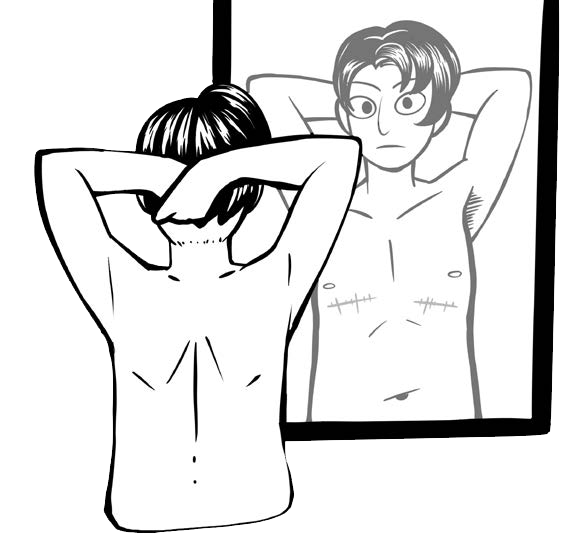
In A Mirror
Look at your breasts/chest with your arms at your sides. Next, raise your arms high overhead.
- Look at the size and shape of each nipple and the tissue around it. Check for swelling, lumps, dimpling (looks like an orange peel), scaly skin, or other skin changes.
- Put your hands on your hips and press firmly to flex your chest muscles. Look for any dimpling, puckering, or changes, particularly on one breast or one side of your chest.
Lying Down
When you lie down, your breast/chest tissue spreads out evenly along the chest wall.
- Place a pillow below your right shoulder and put your right arm behind your head.
- Using your left hand, move the pads of your fingers around your
 right breast/chest in small circular motions covering the entire breast area and armpit.
right breast/chest in small circular motions covering the entire breast area and armpit. - Use light, medium, and firm pressure to feel the different levels of your tissue.
- Squeeze the nipple, check for discharge and lumps.
- Repeat these steps for your left breast/chest.
Contact your doctor or nurse practitioner immediately if you detect any changes or abnormalities on your self-exam.
